HSCI researchers create ON-OFF switches to better control CAR T cell activity
HSCI scientists have created molecular ON-OFF switches to regulate the activity of CAR T cells, a potent form of cell-based immunotherapy that has shown dramatic success in treating some advanced cancers, but which also poses a risk of toxic side effects.
Led by HSCI Principal Faculty member Benjamin Ebert at Dana-Farber Cancer Institute, as well as Marcela Maus at Mass General Cancer Center, the researchers developed switchable CAR T cells that can be turned on or off by giving a commonly used cancer drug, lenalidomide. The researchers designed OFF-switch CAR T cells that could be quickly and reversibly turned off by administering the drug, after which the CAR T cells recovered their anti-tumor activity. Separately, the researchers also reported ON-switch CAR T cells that only killed tumor cells during lenalidomide treatment.
Published in the journal Science Translational Medicine, the approach demonstrates the potential of switchable cell therapies. In the future, they might allow patients and their physicians to use a pill – or not – to tune the amount of CAR T cell activity from day to day, hopefully reducing toxic side effects.
Immunotherapy side effects
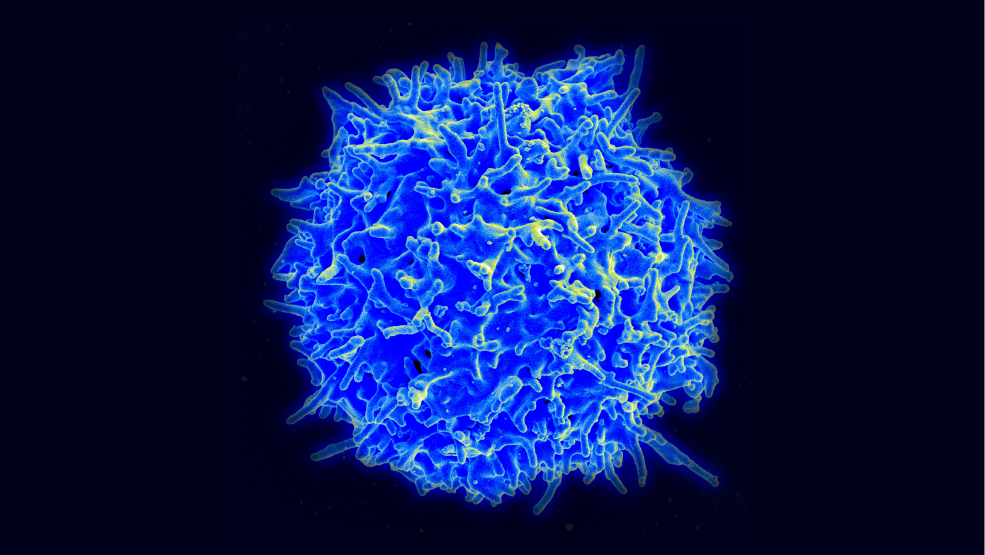
CAR T cells are created by collecting immune T cells from a patient and reprogramming them in the laboratory to produce a finely-tuned receptor molecule, termed a CAR (for chimeric antigen receptor), that recognizes a distinctive protein on the surface of the patient’s cancer cells. The CAR T cells, after being engineered in the lab and returned to the patient, circulate through the body and home in on the cancer cells by binding to the distinctive surface protein they have been engineered to recognize. This binding event stimulates an immune attack, destruction of the cancer cells, and proliferation of the CAR T cells.
A drawback, however, is that uncontrolled proliferation of the CAR T cells sometimes triggers cytokine release syndrome, the release of inflammation-causing signals throughout the body that can cause toxicities ranging from mild fever to life-threatening organ failure. Current management of these toxic reactions relies on intensive care unit support and drugs including immunosuppressive corticosteroids, so many researchers are working on controlling the activity of CAR T cells in order to prevent these potentially lethal side effects.
“CAR T cells can be fantastically effective therapies, but they can also have serious toxicities and can cause significant morbidity and mortality,” said Ebert, who is the Chair of Medical Oncology at Dana-Farber. “They are currently difficult to control once administered to the patient.”
Engineering a molecular switch
To create the ON and OFF switch systems for CAR T cells, the scientists used a technique known as targeted protein degradation. It exploits a mechanism that cells use to dispose of unwanted or abnormal proteins: the proteins are marked for destruction by a structure within cells that acts like a garbage disposal. A small number of drugs, including lenalidomide, act by targeting specific proteins for degradation using this pathway.
The researchers engineered small protein tags that are sent to the cellular garbage disposal by lenalidomide. When this degradation tag was affixed to the CAR, it allowed the tagged CAR to be degraded during drug treatment, thereby stopping T cells from recognizing cancer cells. Because CAR proteins are continually manufactured by these engineered T cells, new CAR proteins accumulate after the drug treatment stops and restore the cell’s anti-tumor function. The researchers propose that the switch system might allow patients to have their CAR T cell treatment temporarily paused to prevent short-term toxicity and still have long-term therapeutic effects against their cancer.
The scientists also built an ON-switch CAR by further engineering the proteins that physically interact with lenalidomide. This system has the potential to be especially safe, because the T cells only recognize and attack tumor cells during drug treatment. If used to treat cancers such as multiple myeloma that are sensitive to lenalidomide, ON-switch CAR T cells could allow for a coordinated attack by the immune cells and the drug that controls them.
The researchers’ approach opens up avenues for developing safer and more targeted cell therapies. Ebert said: “The long-term goal is to have multiple different drugs that control different on and off switches” so that scientists can develop “ever-more complex cellular therapies.”
Read more
This story was originally published on the Dana-Farber Cancer Institute website on January 6, 2021, under the title, “Scientists create ON-OFF switches to control CAR T cell activity.”
Source article: Jan, M. et al. (2020). Reversible ON- and OFF-switch chimeric antigen receptors controlled by lenalidomide. Science Translational Medicine. DOI: 10.1126/scitranslmed.abb6295
This work was supported by the National Institutes of Health, the Howard Hughes Medical Institute, the Edward P. Evans Foundation, and the Leukemia and Lymphoma Society.
