Cancer immunologists and biological engineers at Harvard unite to fight therapy-resistant cancers
A new NIH-funded Immuno-Engineering to Improve Immunotherapy (i3) Center at Harvard University sets out to create new anti-cancer immunotherapies using biomaterials-based approaches. Coordinated by the Wyss Institute of Biologically Inspired Engineering, the collaboration with the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS), Dana-Farber Cancer Institute (DFCI), and Harvard’s Department of Stem Cell and Regenerative Biology brings together world-leading cancer immunology and bioengineering experts to tackle immunotherapy-resistant cancers such as myeloid malignancies and solid tumors.
The Harvard i3 Center is part of NIH’s Cancer MoonshotSM initiative, formed in 2016 to accelerate cancer research, make therapies available to more patients, and improve cancer prevention and early detection.
“We aim to develop new technologies that induce robust anti-cancer T-cell immunity, and we hope that the i3 Center’s highly cross-disciplinary and cross-fertilizing mechanisms will provide a center of gravity for many future efforts in the immunotherapy space across and beyond our collaborating institutions,” said David Mooney, Ph.D., Wyss Institute Founding Core Faculty member and a principal investigator (PI) of the i3 Center.
Mooney is the Robert P. Pinkas Family Professor of Bioengineering at SEAS and leads the Wyss Institute’s Immuno-Materials Initiative. His team uses immune-modulating biomaterials to trigger and enhance T-cell-mediated immune responses against tumors. Together with clinical collaborators, they created the first implantable vaccine to eliminate melanoma tumors in mice – research being taken forward in a Phase I clinical trial at DFCI.
F. Steven Hodi, Jr., M.D., the i3 Center’s other PI, is leading the clinical cancer vaccine trial. Hodi has been at the forefront of developing cancer immunotherapies using “immune checkpoint inhibitors,” a class of drugs that can re-activate tumor-destroying T cells that are otherwise muted in the tumor microenvironment.
“The funding for this center provides a unique opportunity to unite key investigators for translating fundamental advancements in immunology and biomedical engineering into highly synergistic approaches to improve the treatments for cancer patients,” said Hodi, who is Director of Melanoma Center and The Center for Immuno-Oncology at DFCI, and Professor of Medicine at Harvard Medical School.
i3 Projects
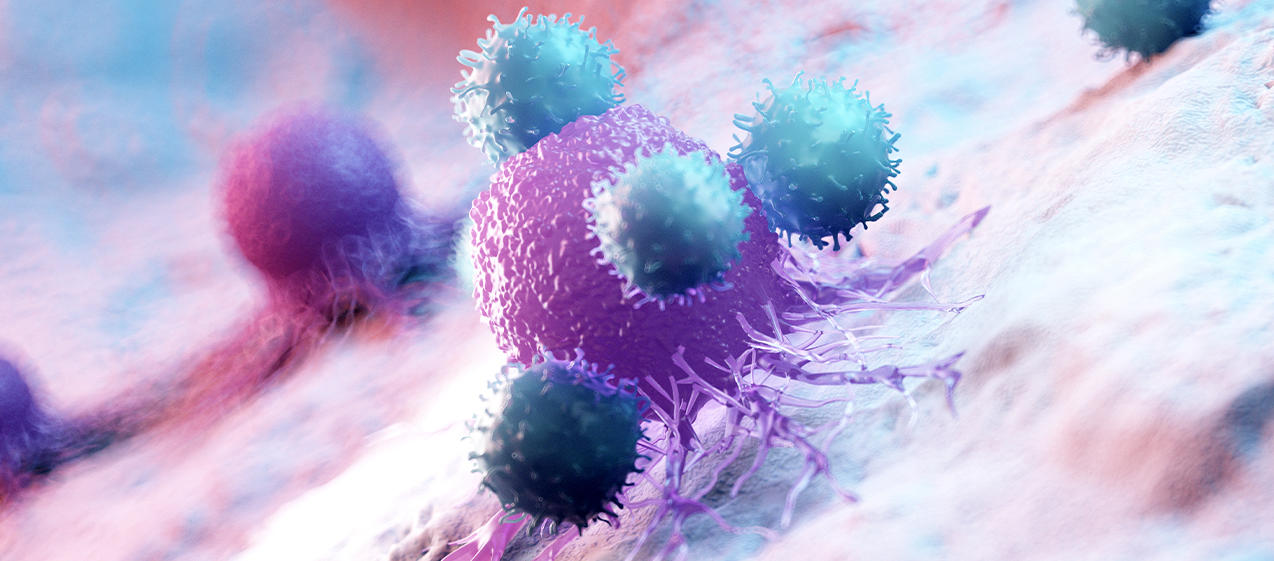
The i3 Center aims to boost tumor-specific activities of cytotoxic T cells. Using both in vivo and ex vivo biomaterials-based approaches, the scientists aim to enhance different stages of the normal process by which T cells develop and acquire anti-cancer activity.
Enhancing anti-cancer immunity
David Scadden, M.D., Professor at Harvard’s Department of Stem Cell and Regenerative Biology, will collaborate with Mooney on an i3 project that builds on their previous work. Scadden and Mooney’s team will engineer biomaterials that recreate key features of the normal hematopoietic stem cell niche in the bone marrow. Such implantable biomaterials could help rapidly amplify T cell progenitor cells, and enhance T cell-mediated anti-cancer immunity. Scadden is the Gerald and Darlene Jordan Professor of Medicine at Harvard University and co-director of the Harvard Stem Cell Institute.
New approaches to T-cell therapy
Some patients are given “adoptive” T-cell therapies, whereby they receive T cells transplants that help them fight their cancer. One i3 project focuses on preparing the T cells prior to transplantation. The investigators plan to develop and test biomaterials that can better mimic normal APCs in activating and directing the function of patient-derived T cells in a dish. This team is led by DFCI researchers Catherine J. Wu, M.D., and Jerome Ritz, M.D. Wu is Chief of the Division of Stem Cell Transplantation and Cellular Therapies, and Ritz is Executive Director of the Connell and O'Reilly Families Cell Manipulation Core Facility at DFCI.
“We need to make efforts to enhance the ability of the immune system to recognize tumor cells. One direction my laboratory is taking makes use of innovative biomaterials to help us to efficiently expand polyclonal tumor-specific functionally-effective T cells ex vivo in a way that can be readily translated to the clinical setting,” said Wu, whose research group investigates the basis of effective human anti-tumor responses and currently focuses on melanoma and acute myeloid leukemia.
DNA origami for cancer vaccines
Another i3 project seeks to create cancer vaccines using “DNA origami”: biocompatible nanostructures composed of DNA. DNA origami could provide significant advantages in presenting tumor-specific antigens and immune-enhancing adjuvants to APCs. It can modulate the concentrations, ratios, and geometries of all components with nanoscale precision, so it can be used to determine configurations that are more effective than other vaccination strategies. The project will be run by Wyss Institute Core Faculty member William Shih, Ph.D., Derin Keskin, Ph.D., lead immunologist at Dana-Farber’s Translational Immunogenomics Lab, and Mooney.
A launchpad for collaboration
With a culture of continuous interaction, sharing of data and samples, and strong expertise provided by senior biostatistician Donna Neuberg, Sc.D., the i3 investigators anticipate the new center will stimulate new research and progress towards new treatments for therapy-resistant cancers.
Source: This is an edited version of an article by Benjamin Boettner that originally appeared on the Wyss Institute website, entitled, "Harvard’s Wyss Institute announces cross-institutional “Immuno-engineering to Improve Immunotherapy (i3)” Center to advance cancer therapy".