HSCI scientists advance Type 1 diabetes therapy by protecting cells from immune attack and stress
The stem cell-based approach to treating Type 1 diabetes (T1D) is successfully being tested in the clinic, using a transplant of stem cell-derived beta cells (SC-beta cells) to give patients their own source of insulin. One challenge in developing the therapy is the cells’ vulnerability to stress and the immune system, which can lead to cell malfunction or death.
A new study, published in the journal Stem Cell Reports, used genetic engineering to improve SC-beta cell survival and function. The research was led by Douglas Melton, the Xander University Professor of Stem Cell and Regenerative Biology at Harvard and the Co-Director of the Harvard Stem Cell Institute.
Sugar levels in the blood increase in response to food intake and are regulated by the hormone insulin, which is secreted by beta cells in the pancreas. In response to glucose, beta cells secrete insulin to make blood glucose levels go down. When beta cells are destroyed or dysfunctional, blood glucose levels rise beyond normal levels.
In patients with T1D, the immune system attacks and destroys beta cells. Patients depend on daily insulin injections, but the challenge of using this treatment to regulate glucose levels means that patients can experience episodes of excessively low or high blood glucose, leading to potential organ damage and shortened lifespan.
A promising alternative to insulin injections is the transplantation of beta cells, which are obtained from deceased organ donors, or more recently, derived from stem cells. Following transplantation, SC-beta cell survival and function critically depends on the cells’ resistance to the body’s immune response and environmental triggers at the transplantation site. Furthermore, stressed beta cells are thought to be even more susceptible to immune attack, so preventing SC-beta cell stress may be critical in the context of T1D.
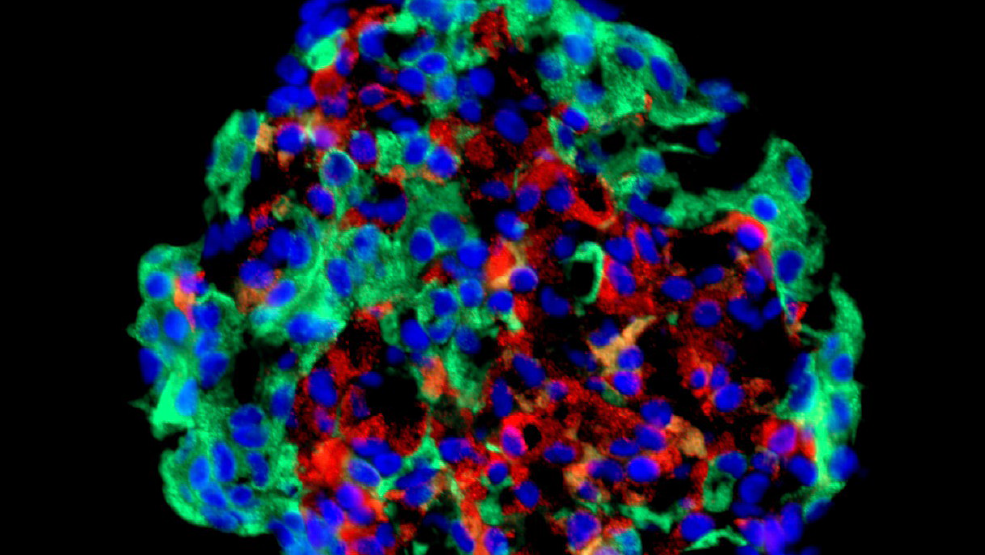
In the study, researchers developed a way to improve SC-beta cell stress resistance and survival. By genetically engineering SC-beta cells, the researchers selectively reduced the levels of four mediators of stress susceptibility and immune cell recognition. As a result, the engineered cells were more resistant to stress from inflammatory molecules or high glucose. They were also less susceptible to being killed by immune cells, showing overall increased survival in lab culture experiments.
Future research will investigate whether the genetic modification of SC-beta cells can permanently protect transplanted cells from immune cell attack or other stressors, without negatively affecting their function or safety properties.
Read more
This story is adapted from a press release published by the by the International Society for Stem Cell Research on March 3, 2022.
