HSCI scientists show that engineered “5-module CAR” T cells target harmful T cells responsible for type 1 diabetes
Researchers have engineered a specialized type of T cell that can specifically target and eliminate harmful T cells, particularly the pathogenic ones that cause type 1 diabetes. In addition to preventing type 1 diabetes, the engineered T cell approach can potentially be applied to other autoimmune diseases, such as multiple sclerosis; certain cancers; and immune rejection of transplanted tissues.
The research was co-led by Thomas Serwold, a Harvard Stem Cell Institute affiliate faculty member at Joslin Diabetes Center, and Michael Kuhns of the University of Arizona College of Medicine in Tucson. The study was published in the Proceedings of the National Academy of Sciences.
In general, chimeric antigen receptor (CAR) T cells are engineered with an artificial receptor that targets the cells responsible for disease. While CAR-T cell therapy has shown clinical success with some B cell lymphomas, the approach has a number of drawbacks including the dosing required, as well as the T cells’ specificity and sensitivity.
To address these issues, the team mimicked natural T cell responses that are driven by a complex “5-module” group of molecules. By designing T cells with this 5-module group (5MCAR), the researchers directed the cells to target and eliminate the pathogenic T cells that destroy pancreatic beta cells and lead to type 1 diabetes.
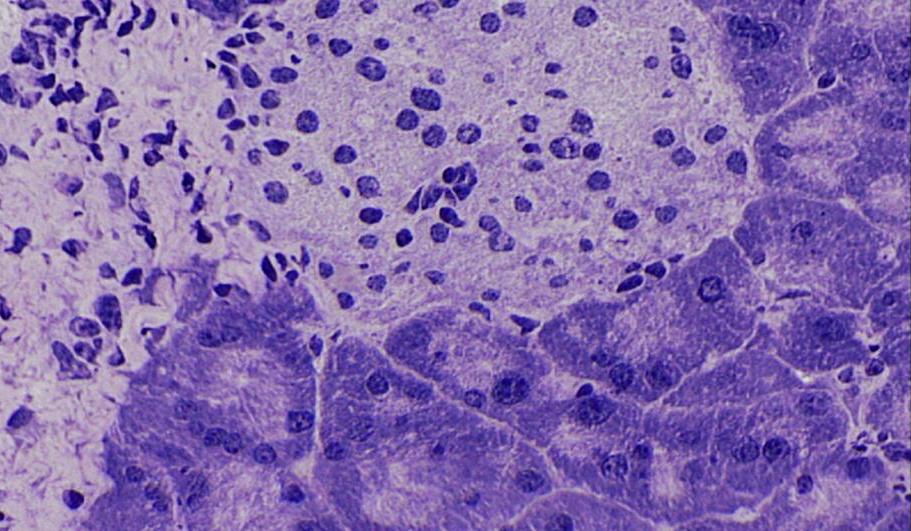
The researchers found that in a mouse model of type 1 diabetes, the 5MCAR T cells could rapidly find and eliminate the other T cell targets and prevent the development of diabetes. In contrast, all untreated mice developed diabetes.
Further experiments showed that the untreated mice had extensive pancreatic damage, as compared to the treated mice. Longer-term experiments established that the 5MCAR T cells could engraft for up to a year following administration, indicating potential for long-term protection.
Kuhns said: “Basic research from labs around the world, including ours, has helped us to understand the complex structure and function of the 5-module molecular machines that have evolved to drive T cell responses. These insights motivated us to ask if we could engineer a biomimetic 5-module CAR that mirrors the form and function of the natural counterpart. We think these results show that a biomimetic approach holds promise for CAR engineering.”
Serwold added: “When we saw that our 5MCAR T cells completely eliminated the harmful T cells that invaded the pancreas, we were blown away — it was like they hunted them down. That ability is why we think that 5MCAR T cells have tremendous potential for treating diseases like type 1 diabetes.”
Read more
This story was originally published on the Joslin Diabetes Center website on November 2, 2020, under the title “5-module CAR-T cells show promise for targeting pathogenic T cells and preventing the development of type 1 diabetes.”
Source article: Kobayashia, S., Thelin, M. A., et al. (2020). A biomimetic five-module chimeric antigen receptor (5MCAR) designed to target and eliminate antigen-specific T cells. Proceedings of the National Academy of Sciences. DOI: 10.1073/pnas.2012495117
This study was supported by the University of Arizona College of Medicine, the BIO5 Institute, the National Institutes of Health, the Pew Scholars Program, the University of Arizona Foundation, the Cancer Center Support Grant, the Fleisher Family Foundation, the Alexander and Margaret Stewart Trust, the Iacocca Family Foundation, the Swedish Society of Medicine, the Swedish Society of Medical Research, Harvard Catalyst, and the Harvard Clinical and Translational Science Center.
