Harvard Stem Cell Institute (HSCI) researchers have engineered stem cells that can deliver a tumor-suppressing and killing molecule to the brain. They tested the therapy in three new mouse models of breast cancer that metastasizes to the brain, and found that it successfully prolonged the lifespan of the mice. The findings are published in the journal Scientific Advances.
“When breast cancer patients get metastasis to the brain, there’s often not much we can do because therapeutics for brain metastatic cancer are scarce,” said Khalid Shah, M.S., Ph.D., an HSCI Principal Faculty member at Brigham and Women’s Hospital. “Given the urgent need and magnitude of the problem, we set out to not only work on the development of a new therapeutic approach, but also to develop it in a way that maximizes the likelihood that our findings will be clinically translatable.”
Approximately 15 to 30 percent of patients with metastatic breast cancer have brain metastasis (BM), with basal-like breast cancer (BLBC) metastasizing to the brain most frequently. The prognosis for BLBC-BM patients is poor, as the blood-brain barrier prevents most therapeutics from reaching the brain. Testing candidate therapies in clinical trials is also challenging because representative animal models are limited.
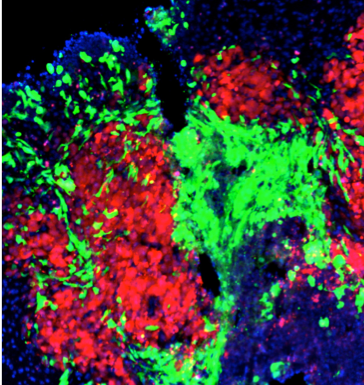
The researchers began their work by analyzing tissue from breast tumors and metastatic tumors in the brain from human patients with BM. They pinpointed key targets that appeared to drive tumor growth: an excess of a growth factor receptor and two cell death receptors. With this knowledge, the investigators genetically engineered a bi-functional molecule to target these receptors simultaneously and induce cell death in the tumors.
Because breast cancer can metastasize to the brain in numerous patterns, the researchers spent three years building mouse models to reflect the range and complexity of human disease. One mouse mimics metastasis that takes the form of a solid tumor in the middle of the brain (macro-metastasis), the second mimics a more scattered metastasis (perivascular niche micro-metastasis), and the third mimics one that appears in the back of the brain (leptomeningeal metastases). Armed with these models, they could more accurately determine the efficacy of the new therapeutic molecule.
To introduce the molecule to the brains, the researchers used a stem cell–based delivery platform because stem cells have the advantage of being able to cross the blood-brain barrier and home to tumors in the brain. In all three mouse models, the researchers observed improved survival rates with the therapy.
“Building these models was essential to testing our therapies because we wanted to mimic what happens in the patients,” Shah said. “We started our research by bringing findings in patients to mice, and now we are planning to go back to the patients.”
The U.S. Food and Drug Administration is currently reviewing a previous iteration of the researchers’ novel therapy, which uses off-the-shelf stem cells to target one of the two receptor types targeted by the new approach. The researchers hope that approval of that therapy might bolster support for the therapy developed in this study.
Read more
This story was adapted from a press release by Brigham and Women’s Hospital, published on March 3, 2021.
Funding for this research was provided by the National Institutes of Health, Overseas Research Fellowships from Uehara Memorial Foundation, and Kanzawa Medical Research Foundation. Shah owns equity in and is a member of the Board of Directors of AMASA Therapeutics, a company developing stem cell–based therapies for cancer.
Source article: Kitamura, Y. et al. (2021). Anti-EGFR VHH-armed death receptor ligand–engineered allogeneic stem cells have therapeutic efficacy in diverse brain metastatic breast cancers. Scientific Advances. DOI: 10.1126/sciadv.abe8671
