HSCI scientists identify stem cell defect as a possible cause of chronic skin disease
Effective targeted therapies have yet to be developed for psoriasis, a skin disorder affecting at least 100 million individuals worldwide. Skin impacted by psoriasis becomes thickened, red, and covered with silvery scales; additionally, changes to patients’ nails and joint deformation can occur.
In a new study, Harvard Stem Cell Institute (HSCI) researchers have uncovered a novel biological pathway that may explain why skin thickens in psoriasis, which could lead to new strategies for developing therapies. Their findings are published in the Journal of Investigative Dermatology.
“Psoriasis places social and psychological stress on patients and is associated with risk of diabetes, cardiovascular disease and more. While steroids and biologics can be prescribed, we don’t have a cure because we haven’t understood the cause,” said co-senior author George Murphy, M.D., professor of pathology at Brigham and Women’s Hospital and co-leader of the HSCI Skin Program. “Our initial finding that skin thickening in psoriasis is due to build-up of dysregulated stem cells and their progeny is exciting because it represents a new way of thinking about an old and significant skin disease.”
Understanding the stem cell defect
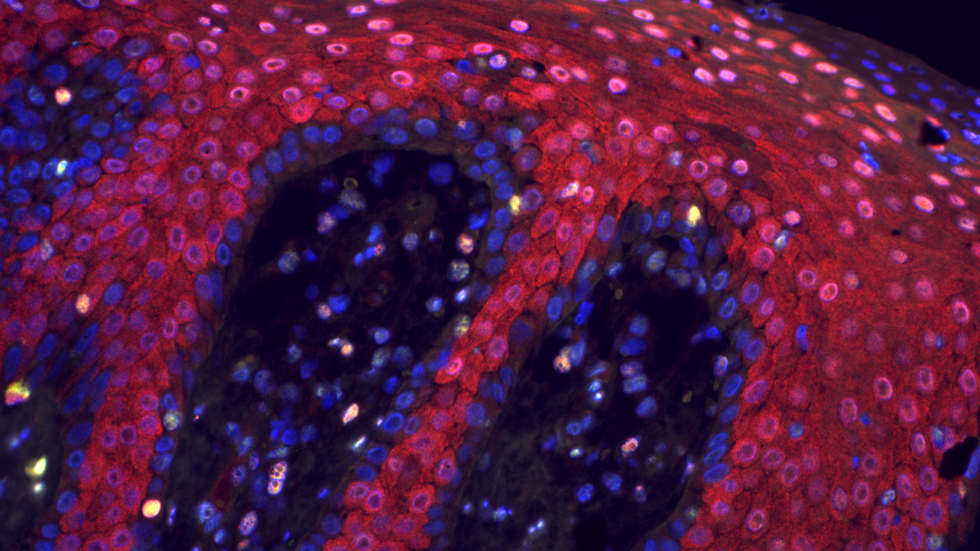
To better understand the basis for the dysregulated skin stem cell behavior, the researchers focused on the epigenome, the molecular wrapping that covers each DNA strand and orchestrates how individual genes behave.
“Without understanding the mechanism underlying a disease, it’s hard to find effective treatments,” said co-senior author Christine Lian, M.D. associate professor of pathology at Brigham and Women’s Hospital. “The question we decided to pursue was: Is there an epigenetic abnormality in psoriasis that may explain why stem cells are misbehaving?”
Lian, Murphy and their colleagues found a defect in the DNA epigenetic covering that resulted in the loss of a particular epigenetic marker known as 5-hmC. The defect was found in cells from patients with psoriasis but not other skin conditions that produce a similar skin thickening, such as callous-like areas from chronic irritation. The team replicated the defect in a mouse model of psoriasis and found that it preferentially affected genes that regulated the function of skin cells.
Correcting the problem
Lian and Murphy have previously shown that 5-hmC loss in the skin epigenome can be reprogrammed using compounds as fundamental as vitamin C. They reasoned that therapeutic correction of the epigenomic defect in psoriasis might reverse the disease process. Based on experiments using skin stem cell cultures in the lab, the team saw promising preliminary results suggesting that 5-hmC levels can be restored to correct the deficiency seen in psoriasis.
While the researchers are interested in how vitamin C can be used, they need to further develop and test effective treatments since simply taking a vitamin supplement would likely have little effect. The team’s next steps involve testing other epigenetic reprogramming compounds on three-dimensional models of skin stem cells.
“If successful, our epigenetic stem cell explanation for psoriasis hopefully could transform therapy, allowing for more personalized and targeted approaches directed at the very cells that accumulate to form the heartbreak of this all-too-often devastating skin condition,” Murphy said.
Discover more
This story was originally published on the Brigham and Women’s Hospital website on December 11, 2019.
Source article: Li, F., Yuan, C. W., et al. (2019). Loss of the Epigenetic Mark, 5-hmC, in Psoriasis: Implications for Epidermal Stem Cell Dysregulation. Journal of Investigative Dermatology. DOI: 10.1016/j.jid.2019.10.016
Funding: This study was supported by the LEO Foundation, the Harvard Stem Cell Institute, and the Department of Pathology at Brigham and Women’s Hospital, the U.S. Department of Defense, and the National Institutes of Health.
