HSCI researchers led by Tracy Young-Pearse, Ph.D., have developed a method to examine living brain cells and predict the rate of Alzheimer’s disease progression and cognitive decline.
A new brain model has been developed that will allow patient-specific insights in Alzheimer’s disease (AD).
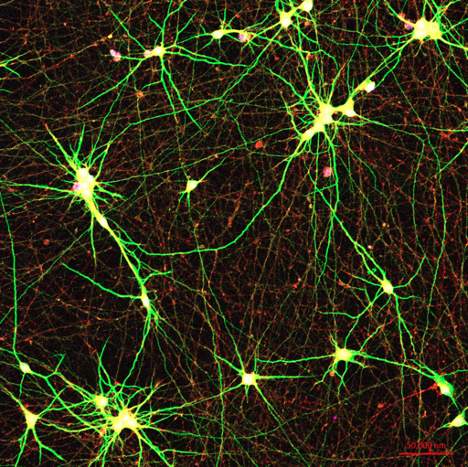
Researchers from Brigham and Women’s Hospital, led by Harvard Stem Cell Institute (HSCI) Principal Faculty Tracy Young-Pearse, Ph.D., have developed a method to examine living brain cells and predict the rate of cognitive decline in humans. In their study, published in Neuron, the team generated induced pluripotent stem cell (iPSC) lines from over 50 individual subjects for whom longitudinal clinical data, quantitative neuropathology data, and rich genetic and molecular profiling of brain tissue were also available. The power of this new resource was demonstrated through a series of studies that turned these stem cells into brain cells and then analyzed molecular pathways active in these living neurons in a dish. Specific forms of amyloid beta-protein (Aβ) and tau protein associated with cognitive decline and AD were identified, which reveal signaling pathways influencing the production of these toxic species.
“We are finding that different genetic backgrounds in humans generate different profiles of Aβ and tau,” said Young-Pearse, an associate professor in the Ann Romney Center for Neurologic Diseases at Brigham and co-leader of the HSCI Nervous System Diseases Program. “Those stem cell-derived neuronal profiles have a predictive nature, in terms of the clinical outcome of an individual’s Alzheimer’s disease. This large set of human cell lines from AD and aged normal people provide the scientific community with a powerful experimental system for untangling why some people develop AD and others do not.”
The study leveraged a large cross-institutional collaborative effort that follows a cohort of people from the Religious Orders Study (ROS) and the Rush Memory and Aging Project (MAP) at Rush University. All individuals entered the ROS and MAP studies with no history of AD or any other neurological diagnosis, but more than one-third went on to develop AD over time. Stem cell lines were generated from blood samples of over 50 of these individuals, who lived to an average of 90 years of age. While the subjects were alive, detailed clinical records and full genome sequencing were collected for each person. After death, the brains of the deceased also were studied and compared to their cultured brain cells in a dish.
The researchers measured Aβ and tau generated by the stem cell-derived neurons and found that specific Aβ and tau species were associated with the levels of plaque and tangle deposition in the brain and the trajectory of cognitive decline.
“If you look across cell culture samples from 50 people, you can predict from the Aβ and tau profiles some features of the cognitive status of that person – their rate of cognitive decline and whether they developed AD – which is absolutely remarkable,” Young-Pearse said.
The authors recognize that, since participants of the ROS and MAP cohorts were primarily Caucasians of European origin, their observations may not be applicable to more diverse populations. The research team has already undertaken the development of 50 new iPSC lines that will be derived from people of color and non-Caucasian groups.
The research team is also exploring if the stem cell-derived neurons can predict whether drugs like aducanumab, a new Alzheimer’s drug recently approved by the Food and Drug Administration, will be more effective in specific groups of AD patients.
“The new Alzheimer’s drug is an antibody that recognizes Aβ and clears it from the brain,” said Young-Pearse. “What our system provides is a platform to test who might be responsive to different AD therapeutics.”
The research team hopes to convey to the public that Alzheimer’s is usually not caused by a single genetic mutation but instead can have different sets of genes contributing to risk across different people.
“There’s a perception that this disease is one uniform disease that shows up and progresses the same way for everyone,” Young-Pearse said. “It’s important to understand that Alzheimer’s is actually quite heterogeneous in its underlying causes, ages of onset and disease course. This is the first time we have a system in place to study living human brain cells from many people to understand better why some develop AD in a very specific way and others are resistant to the disease.”
Read more
See Lagomarsino, VN and Pearse RV et al. “Stem cell derived neurons reflect features of protein networks, neuropathology and cognitive outcome of their aged human donors.” Neuron, Sept. 1, 2021.
This study is part of the AD Deep Phenotyping program supported by a gift from Rick and Nancy Moskovitz. This work also was supported by NYSCF, the Ellison Foundation, the Orchard Foundation, the National Institutes of Health (grants R01AG061894-01, U01AG046170-06, RF1AG057440-01, R01AG055909, R21AG056011, and R21MH118576).