What makes SARS-CoV-2, the virus behind COVID-19, such a threat? A new study by HSCI researchers pinpoints the likely cell types that the virus infects. Unexpectedly, it also shows that one of the body's main immune defenses against viral infections may actually help the virus infect those very cells.
The research was led by Jose Ordovas-Montanes, an HSCI principal faculty member at Boston Children’s Hospital, and Alex Shalek, an HSCI affiliate faculty member at Massachusetts Institute of Technology. The study was published in the journal Cell.
The researcher’s findings will help focus efforts to understand what SARS-COV-2 does in the body, why some people are more susceptible, and how best to search for treatments.
Multiple research models
When news broke about a new coronavirus in China, Ordovas-Montanes and Shalek had already been studying different cell types from the human respiratory system and intestine. They also had gathered data from primates and mice.
In February, they began diving into these data.
"We started to look at cells from tissues such as the lining of the nasal cavity, the lungs, and gut, based on reported symptoms and where the virus has been detected," Ordovas-Montanes said. "We wanted to provide the best information possible across our entire spectrum of research models."
COVID-19-susceptible cells
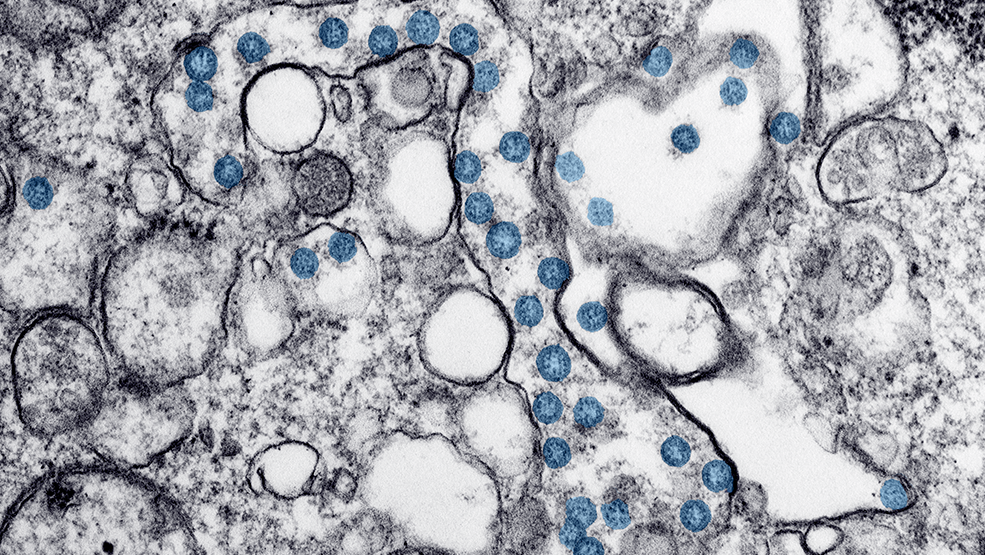
Recent research had found that SARS-CoV-2 uses a human cell receptor called ACE2 to gain entry into cells, aided by an enzyme called TMPRSS2. That led the researchers to ask a simple question: which cells in respiratory and intestinal tissue express both ACE2 and TMPRSS2?
To address this question, the team turned to single-cell RNA sequencing, which identifies which genes are expressed in individual cells. They found that only a small percentage of human respiratory and intestinal cells make both ACE2 and TMPRSS2. Those cells fall in three types: cells in the nose that secrete mucus, lung cells that help maintain air sacs, and cells that line the small intestine and are involved in nutrient absorption.
Data from non-human primates showed a similar pattern of susceptible cells.
“Many existing respiratory cell lines may not contain the full mix of cell types, and may miss the types that are relevant," Ordovas-Montanes said. “Once you understand which cells are infected, you can start to ask: How do these cells work? Is there anything within these cells that is critical for the virus's life cycle?”
He added: “With more refined cellular models, we can perform better screens to find what existing drugs target that biology, providing a stepping stone to go into mice or non-human primates.”
Interferon: helpful or harmful?
In addition to identifying COVID-19-susceptible cell types, the researchers found that the ACE2 gene is stimulated by interferon — one of the body's main immune defenses when it detects a virus. Interferon proteins actually turned the ACE2 gene on at higher levels, potentially giving the virus new portals to get in.
"ACE2 is critical in protecting people during various types of lung injury," Ordovas-Montanes said. "When ACE2 comes up, that's usually a productive response. But since the virus uses ACE2 as a target, we speculate that it might be exploiting that normal protective response."
Interferons are currently being tested as a potential treatment for COVID-19. It is not yet clear whether they might help, or do more harm than good.
"It might be that in some patients, because of the timing or the dose, interferon can contain the virus, while in others, interferon promotes more infection," Ordovas-Montanes said. "We want to better understand where the balance lies, and how we can maintain a productive antiviral response without producing more target cells for the virus to infect."
Community effort
The researchers also want to explore what the virus is doing in the cells it targets, and to study tissue samples from children and adults to understand why COVID-19 is typically less severe in younger people.
"This has been an incredible community effort — not just within Boston, but also with collaborators around the world who have all shared their unpublished data to try and make potentially relevant information available as rapidly as possible," said Shalek. "It's inspiring to see how much can be accomplished when everyone comes together to tackle a problem."
Read more
The original version of this story was published on Boston Children’s Hospital website on April 24, 2020.
Source article: Ziegler, C. G. K., Allon, S. J., Nyquist, S. K., Mbano, I. M., et al. (2020). SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. DOI: 10.1016/j.cell.2020.04.035
