Lee Rubin and Tracy Young-Pearse are uniting HSCI researchers against neurological disease, attacking it from multiple directions.
At some point in our lives, each of us will be affected by neurological disease. That stark reality has motivated scientists in the HSCI Nervous System Diseases Program to join forces to combat diseases like Alzheimer’s, Parkinson’s, autism, and ALS from every direction.
We have known for a long time that the central nervous system (CNS) has an impact on peripheral systems, like the heart. New evidence shows us that the CNS itself is affected by diseases of the blood, metabolism, and heart, as well as by gut microbiota.
To get to the causes of neurological diseases, we need to know about all of these tissues and how they interact.
Our approach to disease
Alzheimer's disease (AD) provides a good example of how we approach disease. Although many therapeutic compounds have been developed to treat AD, none has been found to work in clinical trials. That’s partly because there are so many different factors that contribute to its development and progression.
But there is hope: research shows us that neural tissues damaged by disease, injury, and aging can be repaired. Our program builds on this knowledge. We set aside the notion that there is no way back after the onset of symptoms, and explore how cognitive function can be improved in people already diagnosed with AD.
Alzheimer’s is just one of the diseases we study in our program, but the basic principles hold true for all neurological diseases. By looking at the problem differently, we aim to accelerate progress towards better treatments and cures.
In the blood
The health of the whole body is related to the health of the brain. Exercise, diet, and stress levels all have an impact on cognitive decline with aging, and even a small insult to the body, like a cold or anesthesia, can affect the rate of cognitive decline in neurological diseases.
In older mice, tissues damaged by aging are improved when exposed to younger blood. This exciting observation points to circulating factors in blood that can repair tissues damaged by disease, injury, or aging.
Some of these factors regulate CNS function, even though they are secreted by cells outside the nervous system. Some affect brain vasculature, which is the key interface between the brain and blood-borne factors. Cardiovascular and metabolic diseases have an impact on neurological diseases, while neurological diseases affect blood vessels and the gut.
We cannot ignore these connections.
Our program sets up collaborations between experts in all of the tissues of the body, not just the central nervous system. That’s how we are figuring out the relationship between peripheral tissues and the brain.
Gut feeling
Decades before the onset of Parkinson’s disease, patient records show pathologies in the intestine. For many diseases of the nervous system, chronic constipation is an early warning sign, while CNS symptoms are last to appear. We want to know whether brain symptoms can be prevented by treating these earlier symptoms.
To find out, we investigate where and how these diseases start, and whether mutations in one set of genes has an impact on both the intestine and the brain. Using electronic health records, we look for associations between Parkinson’s disease and earlier health problems to see if we can do better at anticipating risk.
Only human
Studying neurological diseases in mice can reveal promising directions for research. But human and mouse brains are quite different.
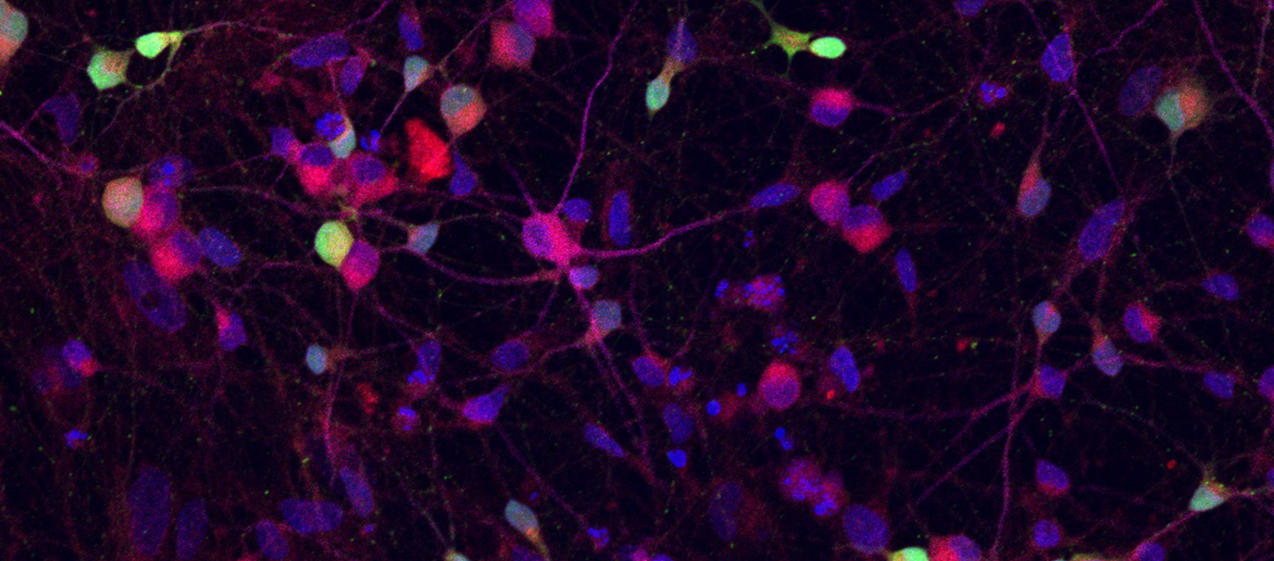
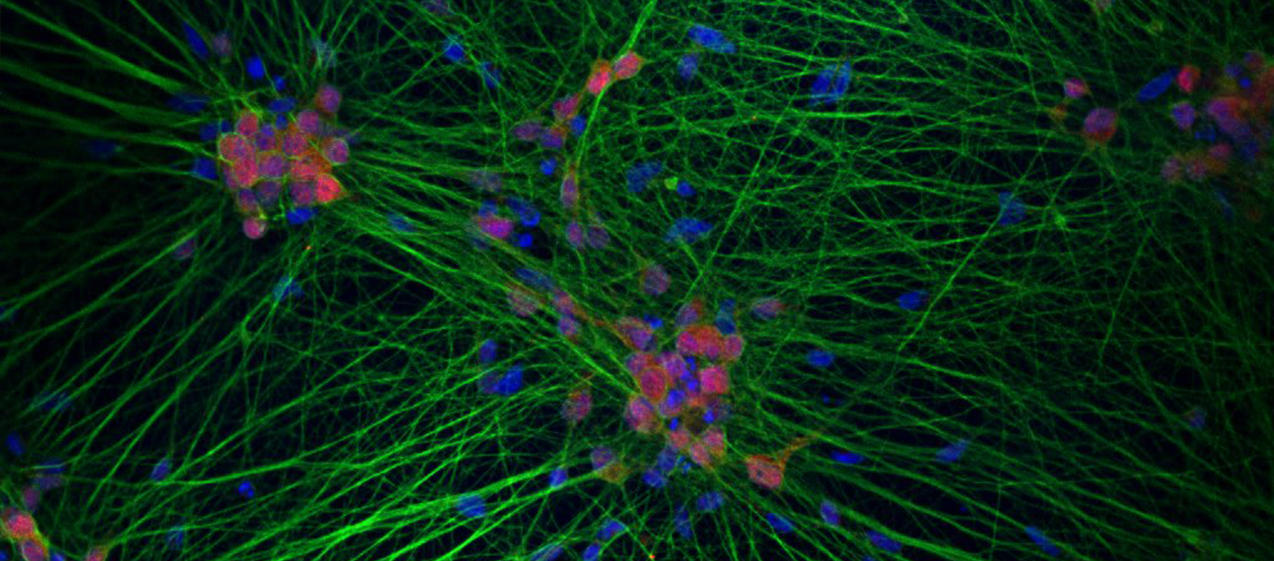
Fortunately, the recent development of human cellular models has transformed neurological disease research. We can now study these diseases in humans by growing neural tissue in a lab from a patient’s own blood or skin cells. That allows us to investigate the effect of potential interventions on Parkinson’s, ALS, Alzheimer’s, and other diseases before testing them on patients.
Collaboration
Our Nervous System Diseases Program includes Harvard scientists with expertise in:
- blood vessel development,
- metabolic disease,
- neurological disease, and
- bioengineering.
We catalyze spontaneous interactions, fund collaborative grants, and encourage co-mentored trainees across laboratories to ensure a healthy flow of ideas, know-how, data, and technology.
We empower our scientists to use the tools they need, including induced-pluripotent stem cells (iPSCs) derived from patient tissues, organoids, organ-on-chip technology, bioimaging, and electrophysiology in living systems. And because the frontiers of science are always moving, we also support the development of new tools to accelerate discovery.
How you can help
By supporting the HSCI Neurological Diseases Program, you will help us achieve our goal of restoring function, not just mitigating impact, in people who are affected by cruel neurological diseases.
You will also help us expand the HSCI network, incorporating new areas of expertise and specialized knowledge into our research. That means supporting the best of HSCI, helping us make the most of the outstanding talent at Harvard and its affiliated hospitals.
| Help us fight nervous system diseases |


