Researchers experiment with single shot that slows rejection
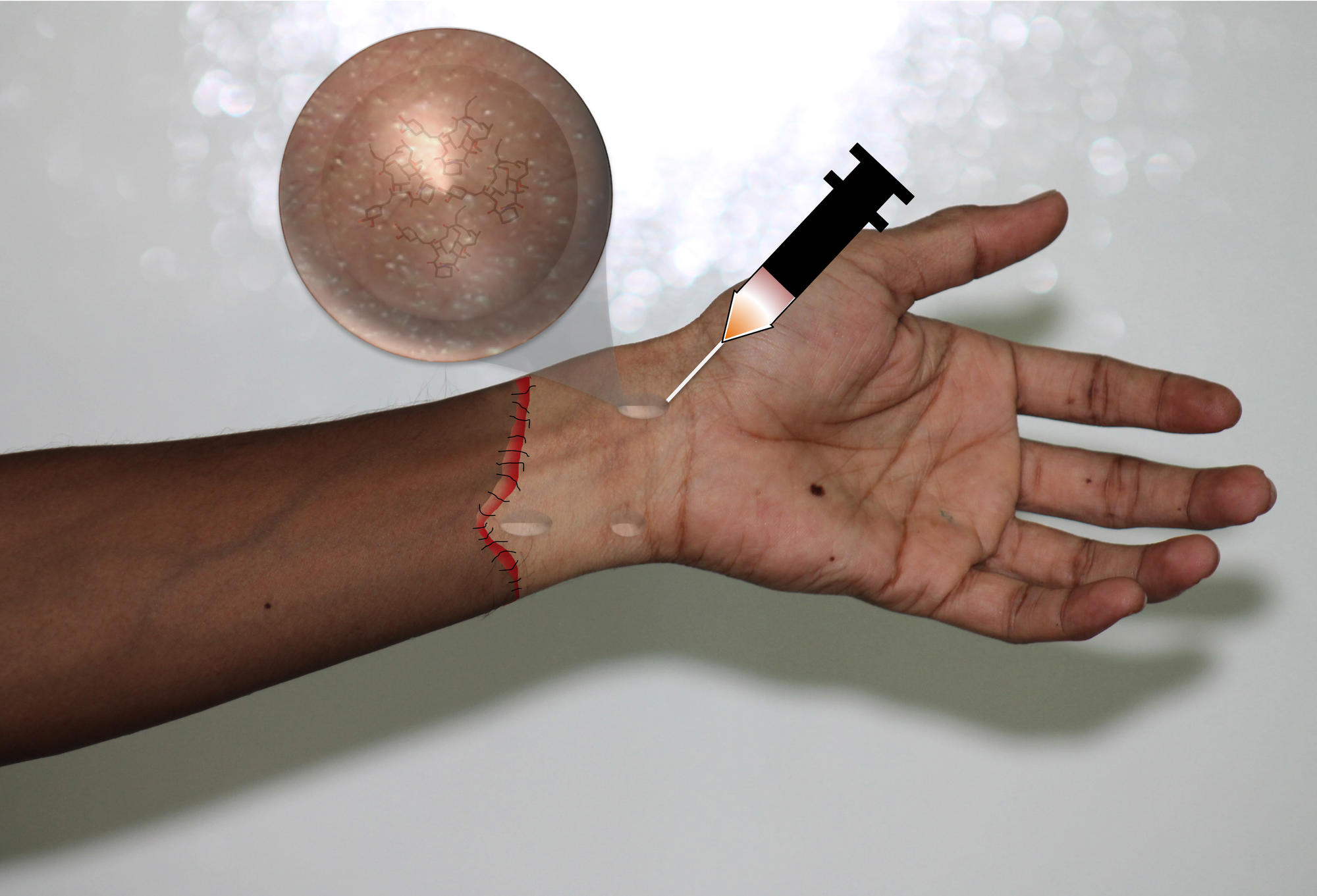
A drug-secreting gel that holds back the immune system—developed to help treat diseases such as brain cancer, ulcerative colitis, and arthritis—has now been shown to slow hand transplant rejection, in rats, when delivered through a single shot. The success may yield a new strategy to improve quality of life for transplant patients who opt to have this complicated, and somewhat controversial, procedure.
Laboratories on three continents collaborated on the project: At Brigham and Women’s Hospital in Boston, bioengineer Jeffery Karp, PhD, developed the gel; at the Institute for Stem Cell Biology and Regenerative Medicine in Bangalore, India, biochemist Praveen Kumar Vemula, PhD, optimized the gel; and at the Bern University Hospital in Switzerland, clinical researcher and surgeon Robert Rieben, PhD, led the in vivo experiments and analyses.
As reported in Science Translational Medicine, a single injection of the immunosuppressant-filled gel allowed rats to live normally with a transplanted limb for over three months, as opposed to just one month with the drug alone. In some cases, a rat could go close to five months without limb rejection, which is when the immune system recognizes the transplant as foreign and begins to completely destroy the tissue.
“This is a proof-of-concept study,” said Karp, who holds faculty positions at the Harvard Stem Cell Institute and the Massachusetts Institute of Technology. “Humans typically take a regimented cocktail of immunosuppressants after a transplant, and so we still need to show that you can entrap different types of drugs—which we’ve done before. But, you could imagine that instead of this cocktail, patients could visit their clinician every six months or so for a shot, which would decrease systemic toxicity, increase compliance, and help prevent missed doses.”
The Karp Lab developed the drug-filled gel used in the shot about five years ago. It was built from small molecules used in ice cream that are easily obtainable and inexpensive. The gel is designed to break down in response to immune system activity, so that as the immune system begins to reject a transplant, the gel dissolves and releases a drug that subdues the immune response. Not all of the dosage is released at once, which allows for longer-lasting protection.
The researchers chose to apply the shot to hand transplants because it could help reduce recipients’ susceptibility to infection from the immunosuppressants. At the moment, the procedure is somewhat controversial, as patients must weigh whether they would rather live under these conditions with a transplanted hand or live with a prosthetic hand.
“Hoping that our work could potentially improve a patient’s quality life has been a major driving force to pursue this research,” said Vermula, who began working on this project as a postdoctoral fellow in the Karp Lab and recently established his own lab at the National Centre for Biological Science’s Institute for Stem Cell Biology and Regenerative Medicine.
“Until now, delivering drugs for the treatment of inflammatory diseases has been extremely challenging due to unpredictable disease severity,” he added. “Hence, our vision is to develop drug delivery systems that release drugs on-demand, in response to the disease severity. I believe this system is a successful first step.”
The global effort that produced the limb transplant work came about when Rieban and his colleagues at the Bern University Clinic of Plastic and Hand Surgery were searching for immunosuppressive treatment options for rat hind limb transplantations. A postdoctoral fellow working in Karp’s lab in Boston, who did his PhD thesis in a neighboring lab at Bern, connected the Bern team to Vemula and Karp.
“The collaboration made us realize that there are more medical conditions with quality-of-life issues our technology could apply to than we ever imagined,” Karp said. “This was an application that was not on our radar and by a chance interaction, we have a project that could one day be helpful to patients, and we’re dedicated to taking these advances as far and as fast as we can.”
“We currently have a ‘BBB’ (Bern-Boston-Bangalore) collaboration and we got ‘AAA’ results,” Rieben said. “We want to keep this rating.”
The research was funded by the American Society for Surgery of the Hand and the Olga Mayenfisch Foundation. Additional support provided by the Julia Bangerter-Rhyner Foundation, the Harvard Institute of Translational Immunology, the Helmsley Charitable Trust, and the National Institutes of Health.
Cited: Vögelin, et. al. A single localized dose of enzyme-responsive hydrogel improves long-term survival of a vascularized composite allograft. Science Translational Medicine. August 13, 2014. DOI: 10.1126/scitranslmed.3008778
(Photo credit: Praveen Kumar Vemula, PhD)