Clifford Woolf wants to reboot drug discovery to find a new way to treat pain: effectively and responsibly.
- Woolf’s goal is to stop the opioid crisis by rejecting the conventional approach to drug discovery and developing painkillers that do not harm people or communities.
- He is using stem cells to create models of pain, outside the body and in a dish, that can be used to screen for drugs swiftly and on a large scale.
- The new approach requires ‘all hands’: expertise, equipment, and collaboration in stem cell biology, genomics, and computer science.
Download a printable version of this story
“I’m going to do my very best to develop non-addictive analgesics – pain killers – to eliminate the need for opioids. I feel that the medical profession, and certainly the pharmaceutical industry, have contributed to the opioid crisis, and we owe it to society to start again and do better,” states Woolf, a soft-spoken man whose warren-like lab is abuzz with activity.
“The World Health Organization refers to ‘the analgesic ladder,’ whereby if you have mild pain, you take a non-steroidal anti-inflammatory, like ibuprofen. If you have moderate pain, you take a mild opioid together with a non-steroidal anti-inflammatory drug. And if you have severe pain, you take a stronger opioid. But this is a stepladder to addiction, overdose and death,” he explains. “I want to change it so that there are no opioids on that ladder at all – and that’s what I’m going to do.”
Starting over
Woolf believes that the traditional approach to drug discovery has taken science down the wrong path.
“I want the pharmaceutical industry to throw away its decades-long approach to drug discovery and start again. The standard approach is to identify a single molecular target – one protein, for example – that is associated with a disease, and test millions of compounds against it until you find one that blocks it and changes the outcome.
“The industry has invested billions of dollars in this approach, but the success rate is not great. And I think where it’s gone wrong is the failure to recognize that single targets are not diseases, especially complex conditions like pain.”
Embrace the complexity
Rather than trying to target single molecules, Woolf thinks we could be harnessing our new knowledge of cell types to screen for drugs.
“To find drugs that act only on diseased cells, we need a much better understanding of all the cell types in the body – what they do physiologically, and how each of them changes over time and, moreover, in disease conditions. Stem cell technology is allowing us to embrace this complexity.”
Stem cells: not just for therapy
Woolf and his fellow HSCI faculty member Paola Arlotta use stem cells to model disease and create tools for discovery. These tools include the specific cells involved in particular diseases, such as the first set of sensory neurons to trigger pain. “People normally think of stem cells as treatments. But Paola is using them to create complex, networked-based models of human neuronal disease that we can use in research.”
Arlotta studies assemblies of cells, called organoids, that mimic brain development. These organoids contain complex circuits, which appear to be disrupted in psychiatric disorders.
“I study the particular neuron that is altered in sensory or motor neuron disorders, so that we can screen for drugs on a large scale,” explains Woolf. “We can take cells from patients as a starting point, change them into stem cells, and use these to make and study human neurons in a dish.”
Woolf wants to use neurons derived from stem cells to screen for drugs that treat pain.
“We can study the protective pain evoked by noxious stimuli, use genetic engineering to mimic the pain produced by genetic mutations, and recapitulate features of the pain that results from inflammation or nerve injury.
“By screening pain in a dish, we hope to find novel solutions to the problem of opioid addiction much more quickly. I believe this approach will give companies a new way to discover medicines that benefit both individual people and their families.”
Human models of disease
So how can you model something like pain, which is so difficult to pin down? Can you observe changes in the properties of neurons in a dish, and screen for drugs that act on those changes?
Woolf thinks it’s definitely possible, at least for some features of pain. Beyond that, he says, we need to look at pain-related circuits.
“Paola is developing organoids that represent the brain and its circuitry. This offers the possibility of studying the circuits responsible for sensations like pain. When she can look at disease-related changes happening in a specific set of cells in those organoids, she will have made a real breakthrough,” says Woolf.
“This is so important for neuroscience, where promising research in animal models has so rarely translated into effective treatments. We need human models of human diseases.”
Machine learning
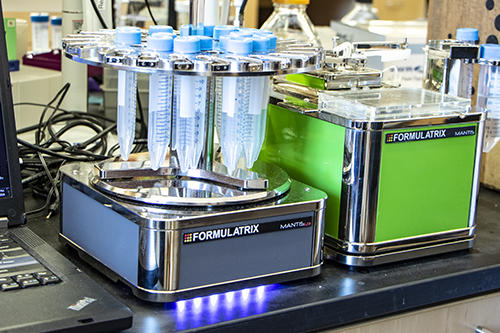
Once pain-receptor neurons can be produced perfectly, they will be used to screen for compounds that act only on specific neurons. That’s one way to generate drugs that act only on diseased cells.
“The more pain-related cells we can make, the better. We can then run genome-wide screens to find which genes contribute to the pain phenotype and which ones suppress it. Big data and machine learning can help here,” says Woolf.
In 2017, Woolf’s team had the resources to hire a dedicated software developer for the first time. Since then, they’ve been using machine learning to train computers to recognize patterns that people can’t see and find clues about what they mean.
“There has been a profound philosophical change in the way science is done. We can now design our experiments to capture the full range of possibilities, because we can screen an entire genome routinely and explore the impact of every gene on a particular function, like pain or neurodegeneration. We are no longer limited by our current knowledge, which is often imprecise and too little.
“We now use image-recognition software to interpret patterns as a cell grows in a dish. It is a much better way to see whether it’s undergoing some neurotoxic process that will kill it.”
‘Big data’ methods do take time: an experiment like this might take several years to set up perfectly, a few days to run, and then another year to analyze. But there is a payoff: they light up the path to knowledge, and point the way to therapeutic success.

What it will take
Reinventing drug discovery is no trivial matter. To achieve their goals, HSCI’s Nervous System Diseases Program needs to create human neurons from stem cells; make induced-pluripotent stem cell lines from patients and keep them alive; set up meticulous, multi-disciplinary experiments; adapt new technologies; write new algorithms; analyze terabytes of multi-layered data; and apply quality control every step of the way.
“Stem cell technology and science are advancing so quickly that having a real impact on patients is within reach. That is very exciting, because there is enormous clinical need,” says Woolf.
“HSCI makes a material difference in the way we operate. It brings people from different sectors together to exchange ideas and helps us form new collaborations between academics and companies, embracing technologically driven opportunities. That is the way real change is going to take place, and how we will ultimately deliver value to patients and society.”
Further information
Download a printable version of this story
