 Harvard Stem Cell Institute researchers at Massachusetts General Hospital (MGH) succeeded in using reprogrammed human stem cells to make working blood vessels in mice that can survive for as long as nine months. The blood vessels were created with induced pluripotent stem cells (iPSCs) derived from the mature skin cells of both healthy adults and individuals with type 1 diabetes.
Harvard Stem Cell Institute researchers at Massachusetts General Hospital (MGH) succeeded in using reprogrammed human stem cells to make working blood vessels in mice that can survive for as long as nine months. The blood vessels were created with induced pluripotent stem cells (iPSCs) derived from the mature skin cells of both healthy adults and individuals with type 1 diabetes.
The research was published in PNAS Early Edition.
"This shows that endothelial cells derived from human iPS lines can form functional and long-lasting blood vessels,” said Laurence Daheron, PhD, Head of HSCI’s iPS Core Facility who helped create the iPSCs. “This could be an approach to treat patients with cardiovascular diseases in the future.“
The ability to regenerate or repair blood vessels could be used in the treatment of cardiovascular disease and other conditions that lead to blood vessel damage, such as diabetes. In addition, supplying blood to newly generated tissue remains one of the greatest barriers to building solid organs through tissue engineering.
The MGH team, co-led by study senior authors Rakesh Jain, PhD, and Dai Fukumura, MD, PhD, of the Steele Laboratory for Tumor Biology, generated the blood vessels by sorting out iPSCs that expressed three protein markers found in cells with the potential to form vasculature. The researchers implanted these cells onto the surface of the brains in muce, along with structural precursor cells, to test their capacity to generate functional blood vessels.
HSCI Co-director David Scadden, MD, visiting scientistf Richard Schäer, MD, and former graduate student Christa Buecker also are co-authors on the paper.
The researchers reported that within two weeks, the implanted cells had formed networks of blood-supplying vessels that appeared to function as well as adjacent natural vessels and continued to function for as long as 280 days in the living animals. While implantation of the same combination of cells under the skin of the animals also generated functional blood vessels, it required implantation of five times more cells, and the vessels were short-lived.
Vasculature-forming cells derived from patients with type 1 diabetes were also successfully used to generate functional, long-lasting blood vessels. However, the researchers noted, different lines of iPSCs from people with diabetes – including different lines derived from the same patient – showed differences in cell-generating potential, indicating the need to better understand the underlying mechanisms.
"The potential applications of iPSC-generated blood vessels are broad – from repairing damaged vessels supplying the heart or brain to preventing the need to amputate limbs because of the vascular complication of diabetes," said co-lead author Rekha Samuel, MD, formerly of the Steele Laboratory and now at the Christian Medical College, Vellore, India. "But first we need to deal with such challenges as the variability of iPSC lines and the long-term safety issues involved in the use of these cells, which are being addressed by researchers around the world."
Support for the study includes grants from the Harvard Stem Cell Institute and the National Institutes of Health.
Shan Liao, PhD, Trupti Vaedam, PhD, Walid S Kamoun, PhD, Ana Batista, PhD, Xiaoxing Han, PhD, Patrick Au, PhD, and Dan Duda, DMD, PhD, of the Steele Laboratory, also contributed to this research.
Adapted from Massachusetts General Hospital press release.
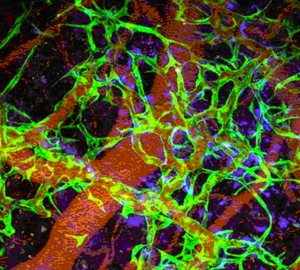
Photo: Laser microscopy image shows iPSC-generated endovascular cells in green, connective tissue cells in blue and red blood cells in red. (PNAS/doi/10.1073/pnas.1310675110)
