Adding two small molecules to mouse iPS cell recipe grows colonies in 48 hours
Harvard Stem Cell Institute scientists at Massachusetts General Hospital have found that adding two small molecules to the four classic “Yamanaka factors” generates the fastest mouse induced pluripotent stem (iPS) cells ever reported. This simple tweak to the iPS cell recipe, published in Nature Methods, yields colonies in as little as 48 hours of factor expression—a great improvement to the 2-4 week wait typical of other protocols. The existence of a more efficient way to generate mouse iPS cells is also evidence that human iPS cell production could similarly be improved.
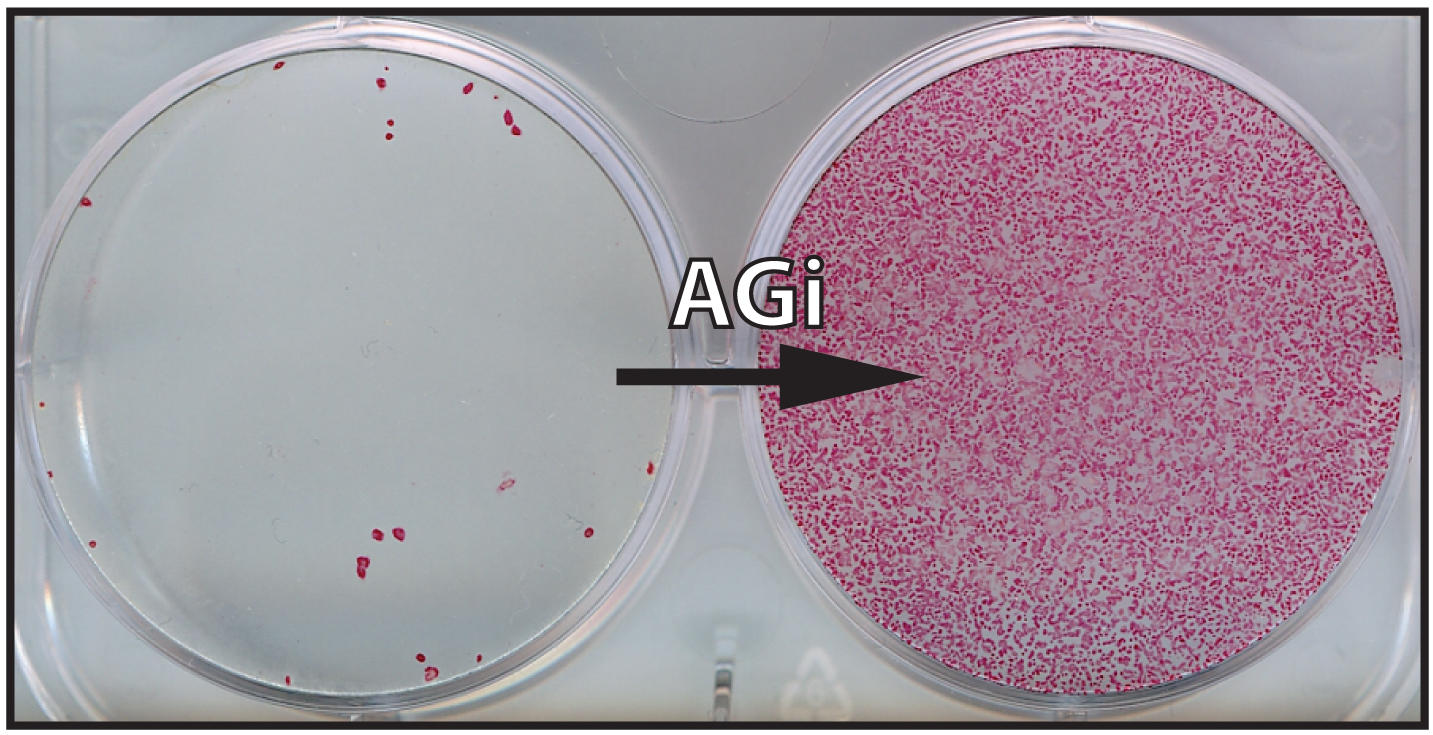
Laboratories have been fiddling with Dr. Shinya Yamanaka’s classic recipe for iPS cells since its publication in 2006. The four “Yamanaka factors”— OCT4, KLF4, SOX2, and c-MYC—are enough to remove the genetic roadblocks that prevent a fully differentiated cell from suddenly changing back into a stem cell, but the process is time-consuming and has about a one in a hundred chance of success. These low odds for producing iPS cells add time and costs to basic research and have become an accepted frustration in the stem cell community.
“We asked ourselves, ‘Why is reprogramming mature cells into iPS cells so inefficient, and can we improve the process in order to better understand the underlying mechanisms and for potentially therapeutic purposes?’” said study senior author Konrad Hochedlinger, PhD, a member of the Massachusetts General Hospital Center for Regenerative Medicine.
Hochedlinger and postdoctoral research fellows Ori Bar-Nur, PhD, and Justin Brumbaugh, PhD, set out to solve this problem by combining different factors known to facilitate reprogramming and screening for which yielded the most successful enhancement of mouse iPS cell formation. The best combination that resulted from the screen was the classic “Yamanaka factors” plus two small molecules, ascorbic acid (vitamin C) and CHIR-99021 (an inhibitor of the GSK3-beta signaling pathway—used in cell-to-cell communication).
“We looked for combinations of factors that would have a synergistic effect,” said Hochedlinger, who is a professor in the Harvard Department of Stem Cell and Regenerative Biology and a Howard Hughes Medical Institute early career scientist. “Both of these molecules have been shown to enhance the formation of iPS cells to some extent in different assays, but what we found is that, when combined, they increase the effectiveness of iPS cell formation by an order of magnitude. It was really a dramatic phenotype to observe.”
This protocol will now help the Hochedlinger Lab grow more quickly the iPS cells they need to study questions related to the stability of cell fate and identity, which are relevant to the field of cancer. The lab is also interested in studying reprogramming in order to change cell fate in more targeted and therapeutically relevant ways. And although preliminary results show that this treatment does not have the same effect in reprogramming human iPS cells, if a similar recipe that boosted their efficiency was discovered, patient stem cell-derived therapies could be much more feasible.
Hochedlinger’s work was supported by, the US National Institutes of Health, the Howard Hughes Medical Institute, a Tosteson & Fund for Medical Discovery award, and a Gruss-Lipper postdoctoral fellowship.
Cited: Bar-Nur, O., and Brumbaugh, J., et al. Small molecules facilitate rapid and synchronous iPSC generation. Nature Methods. Published online September 24, 2014. DOI: 10.1038/NMETH.3142