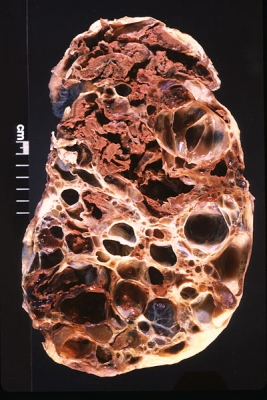
 Harvard Stem Cell Institute (HSCI) scientists have identified a new therapeutic approach for treating polycystic kidney disease (PKD), one of the most common life threatening, inherited diseases in humans, affecting more than 1 in 500 individuals. Patients with the disease experience an abnormal proliferation of kidney cells that ultimately results in cysts and a decline in organ function leading to kidney failure.
Harvard Stem Cell Institute (HSCI) scientists have identified a new therapeutic approach for treating polycystic kidney disease (PKD), one of the most common life threatening, inherited diseases in humans, affecting more than 1 in 500 individuals. Patients with the disease experience an abnormal proliferation of kidney cells that ultimately results in cysts and a decline in organ function leading to kidney failure.
PKD comes in two forms. Autosomal dominant polycystic kidney disease (ADPKD) develops in adulthood and is quite common, while autosomal recessive polycystic kidney disease (ARPKD) is rare but frequently fatal. ADPKD is caused by mutations in either of two proteins, polycystin-1 and polycystin-2, while ARPKD is caused by mutations in a protein called fibrocystin. There is no cure or widely adopted clinical therapy for either form of the disease.
The mechanisms that cause cysts to form have long been poorly understood because doctors can’t routinely remove scientifically useful amounts of diseased cells from patients. Instead, a team of scientists from the HSCI Kidney Disease Program at Brigham and Women's Hospital were able to reprogram the skin cells from five PKD patients—three with ADPKD and two with ARPKD—into induced pluripotent stem cells, which can give rise to many different cell types, and then differentiate them into other cell types.
Led by HSCI Executive Committee member Joseph Bonventre, MD, PhD, and his colleagues Benjamin Freedman, PhD, and HSCI Affiliated Faculty member Albert Lam, MD, the research team examined the patient-derived cells under the microscope, and discovered that the polycystin-2 protein traveled normally to the cilia in cells from ARPKD patients, but did not in ADPKD patients.
Since cells from these ADPKD patients had different mutations in the gene that encodes polycystin-1, as confirmed by collaborators at the Mayo Clinic, the investigators explored the relationship between polycystin-1 and polycystin-2 and found that the mutated polycystin-1 was not able to shepherd the polycystin-2 protein to the cilium to an extent seen in normal cells carrying normal polycystin-1.
"When we added back a healthy form of polycystin-1 to cells, it traveled to the cilium and brought its partner polycystin-2 with it, suggesting a possible therapeutic approach for PKD," explained Freedman in a press release. "This was the first time induced pluripotent stem cells have been used to study human kidney disease where a defect related to disease mechanisms has been found."
The scientists next plan to use a “clinical trial in a dish” approach to identify therapeutics that potentially may never have been considered before for kidney disease. The procedure works by screening a library of small molecules using the patient-derived stem cells to see which of the compounds can facilitate polycystin-2 movement to the cilium, a possible approach to the prevention of cyst growth in people with ADPKD.
“Since you have the abnormalities in the cells, you could potentially try different therapeutic agents that could correct that abnormality, providing a rationale for trying those therapeutic agents first in experimental animals and then potentially in people,” Bonventre said.
The research was funded by the Harvard Stem Cell Institute, the National Institutes of Health, and the March of Dimes. The iPS cells were created with the help of Laurence Daheron, PhD, and her team at the HSCI iPS Core Facility.
Research Cited: Reduced ciliary polycystin-2 in induced pluripotent stem cells from polycystic kidney disease patients with PKD1 mutations. Journal of the American Society of Nephrology. September 5, 2013
Photo: Polycystic kidney (Credit: Ed Uthman/Flickr)
Adapted from American Society of Nephrology press release.
