New culture system makes it possible to observe progression of plaques and tangles
 Massachusetts General Hospital (MGH) scientists, in collaboration with Harvard Stem Cell Institute (HSCI) researchers, have developed a three-dimensional laboratory culture system that can reproduce the full course of events underlying the progression of early-onset familial Alzheimer's disease. Using this system, investigators provide clear evidence supporting the hypothesis that deposition of beta-amyloid plaques in the brain is the first step in a cascade leading to the devastating neurodegenerative disease.
Massachusetts General Hospital (MGH) scientists, in collaboration with Harvard Stem Cell Institute (HSCI) researchers, have developed a three-dimensional laboratory culture system that can reproduce the full course of events underlying the progression of early-onset familial Alzheimer's disease. Using this system, investigators provide clear evidence supporting the hypothesis that deposition of beta-amyloid plaques in the brain is the first step in a cascade leading to the devastating neurodegenerative disease.
"Originally put forth in the mid-1980s, the amyloid hypothesis maintained that beta-amyloid deposits in the brain set off all subsequent events—the neurofibrillary tangles that choke the insides of neurons, neuronal cell death, and inflammation leading to a vicious cycle of massive cell death," said Rudolph Tanzi, PhD, director of the MGH Genetics and Aging Research Unit and co-senior author of the report, which appears in Nature. "One of the biggest questions since then has been whether beta-amyloid actually triggers the formation of the tangles that kill neurons. In this new system we've been able to show for the first time that amyloid deposition is sufficient to lead to tangles and subsequent cell death."
While the mouse models of Alzheimer's disease that express the gene variants causing the inherited early-onset form of the disease do develop amyloid plaques in their brains and memory deficits, the neurofibrillary tangles that cause most of the damage do not appear. Other models succeed in producing tangles but not plaques.
Human stem cell models of early-onset familial Alzheimer's also exist. Earlier this year, HSCI Affiliated Faculty member Tracy Young-Pearse, PhD, of Brigham and Women's Hospital became the first to successfully convert skins cells from patients with early-onset Alzheimer's into neurons that express the disease.
"The work of the Tanzi and Kim labs is remarkable in that they are able to observe two major pathological hallmarks of Alzheimer's disease progression," said Young-Pearse. "In our work, we were able to recapitulate what we believe to be the initiating events in familial Alzheimer's, namely, an increase in toxic amyloid production, and an effect of these amyloid proteins on tau. We did not observe the late stage phenotypes of plaques and tau tangles in our culture system."
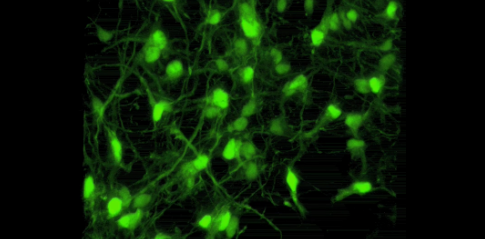
Genetics and Aging Research Unit investigator Doo Yeon Kim, PhD, co-senior author of the Nature paper, realized that the liquid two-dimensional systems usually used to grow cultured cells poorly represent the gelatinous three-dimensional environment within the brain. Instead the MGH team used a gel-based, three-dimensional culture system to grow human neural stem cells that carried variants in two genes—the amyloid precursor protein and presenilin 1—known to underlie early-onset familial Alzheimer's disease. Both of those genes were co-discovered in Tanzi's laboratory.
After growing for six weeks, the neural stem cells expressing the Alzheimer's genes were found to have significant increases in both the typical form of beta-amyloid and the toxic form associated with Alzheimer's. The cells also contained the neurofibrillary tangles that choke the inside of nerve cells causing cell death. Blocking steps known to be essential for the formation of amyloid plaques also prevented the formation of the tangles, confirming amyloid's role in initiating the process.
"This new system—which can be adapted to other neurodegenerative disorders— should revolutionize drug discovery in terms of speed, costs, and physiologic relevance to disease," says Tanzi. "Testing drugs in mouse models that typically have brain deposits of either plaques or tangles, but not both, takes more than a year and is very costly. With our three-dimensional model that recapitulates both plaques and tangles, we now can screen hundreds of thousands of drugs in a matter of months without using animals in a system that is considerably more relevant to the events occurring in the brains of Alzheimer's patients."
"This is an exciting example of the enormous power and opportunity provided for neurological disease modeling and drug screening using stem cell technology,” said study co-author Clifford Woolf, MD, PhD, a neurologist at Boston Children's Hospital and co-leader of HSCI's Nervous System Diseases Program. "We were delighted to contribute to the functional phenotyping of the derived neurons in the 3-D culture as part of an established collaboration with our colleagues in the MGH Department of Neurology."
Cited: Choi, SH, et al. A three-dimensional human neural cell culture model of Alzheimer’s disease. Nature. October 12, 2014 (published online). DOI: 10.1038/nature13800
Adapted from a Massachusetts General Hospital press release by Sue McGreevey.